New innovations are around the corner.
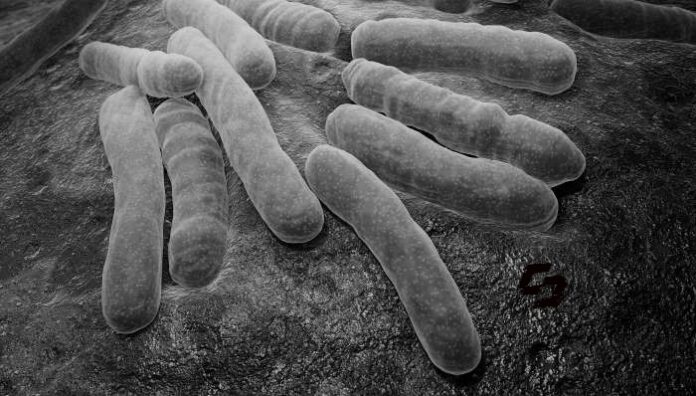
Tuberculosis (TB) is an ancient disease that has proven intractable even in recent decades—but that may be about to change. Watch as Puneet Dewan, senior program officer at the Gates Foundation, reveals some of the most exciting innovations in the R&D pipeline that could transform life for people with TB.
Each year, about 1.6 million people die from TB. That’s even more deaths than from HIV and malaria combined. A disproportionate number of those people live in low- and middle-income countries. There’s only one vaccine for TB, and it’s over 100 years old.
Progress against TB has been slow. But now the world is poised to turn the tide in this fight, thanks to new innovations that may dramatically transform how TB is detected, treated, and prevented.
The world had always said that even if you had a [TB] vaccine, it wouldn’t matter because you couldn’t vaccinate the world’s population for an infectious disease, right?
The other thing that’s super important right now is the BPaL regimen, so-called for MDR TB treatment. MDR TB treatment for those who have rifampicin resistant TB, regular treatment won’t work, and you need more drugs. Previously, injections, super costly, 3,000 pills over two years, with six months of daily injections. I mean, just hell, okay? And it will only work three-quarters time, if you took all your meds.
Now you’ve got a handful of pills a day for six months. Equivalent, a little harder, but equivalent to standard treatment that could be even decentralized out to regular clinics. It’s like, oh, you’ve got TB. Is it this treatment, the treatment A box or the B box for your treatment? And if it’s MDR, now you get the B box. That’s now being rolled out globally with incredible enthusiasm and demand.
This is sort of the intermediate early dividend of all that drug development research is a much cheaper, easier MDR treatment regimen, and that’s going to really transform the lives of those hundreds of thousands of people who have drug resistant TB today. That’s happening now with enormous scale-up globally and that’s a direct outcome of the research and development investment towards that simple, shorter, safer regimen.
What keeps me going ultimately is seeing those systems change, seeing how a country moves from neglecting a disease to tackling it head on and making it a priority, seeing how much fewer children, for example, are actually getting things like TB meningitis, communities of TB survivors are mobilizing to counsel other communities of TB survivors, and actually taking on the responsibility for seeing that they sustain their treatment. Those are the things that really keep you going.