[ad_1]
Would you pay extra to enhance your medical screening with artificial intelligence? In a recent study, more than 30% of women opted for AI-enhanced mammograms—and the results are in.
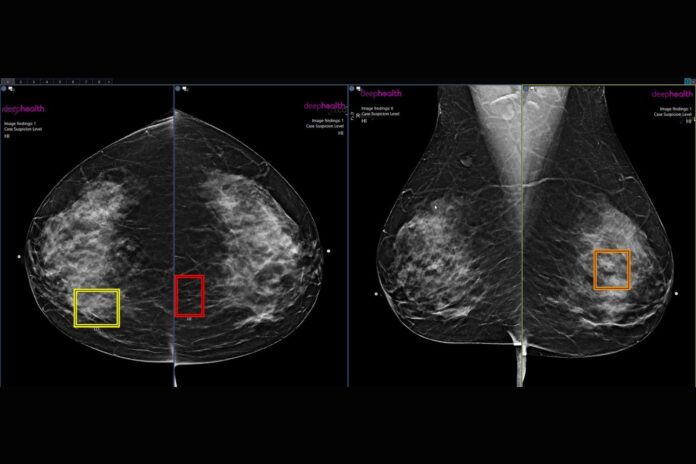
Researchers at this year’s annual meeting of the Radiological Society of North America (RSNA) have revealed that cancer was 21% more likely to be detected for women who paid extra for an AI-enhanced breast cancer screening program. Their findings, presented at the annual meeting and detailed in an RSNA statement, affirm AI’s potential to be a “second set of eyes” for radiologists.
“This is the first report on results from a program that provides an AI-powered enhanced review that patients can elect to enroll in,” Bryan Haslam, chief product officer at DeepHealth who led the study, said in the statement.
The study considered 10 clinical practices offering patients a self-pay, FDA-compliant AI-powered screening mammography program. The X-rays of women who opted into the program were reviewed by a breast radiologist and then by the AI software. If the reviews were inconsistent with each other, a second radiologist would provide a third review.
“The AI-driven enhanced review program leverages AI in a novel workflow to ensure women with suspicious findings get expert level care that could help detect many more breast cancers early,” Haslam added. “The number of women electing for this program is now at 36% and growing, and the rate of cancer detection continues to be substantially higher for those women.”
In fact, of the 747,604 women who had mammograms over a year, the cancer detection rate was about 43% higher for those enrolled in the program compared to those who weren’t. The researchers noted a higher rate at all 10 practices in the study. While they attribute 22% of that increase to the fact that women with a higher risk of getting cancer were more likely to enroll in the program, the remaining 21% of the detection increase came from the AI.
Accordingly, enrolled women were called back for additional screening at a 21% higher rate than unenrolled women, and their positive predictive value for cancer (the chances that positive results for cancer really indicates cancer) was also 15% higher, “indicating that each recall resulted in more cancer diagnoses in the enrolled population,” the researchers wrote. In other words, the recalls triggered with AI help were more accurate.
“These data indicate that many women are eager to utilize AI to enhance their screening mammogram, and when AI is coupled with a safeguard review, more cancers are found,” said Gregory Sorensen, also from DeepHealth and senior writer on the study. Next, the scientists hope to further their research and eliminate the biases that result from self-selection through randomized controlled trials.
These results highlight the potential of AI-enhanced radiology. While some clinics offer the enhancement at an additional cost, the fact that insurances are currently unwilling to cover said cost might be slowing its integration, according to the researchers.
It remains to be seen whether further research will usher in a more widespread and potentially revolutionary use of AI in the diagnostic field, and whether insurance companies will get with the program.
[ad_2]
Source link